Penn Team Makes Inroads Into Reducing Toxicity Associated With Lou Gehrig’s Disease

In a new study published in Nature Genetics, University of Pennsylvania researchers and colleagues have made inroads into the mechanism by which amyotrophic lateral sclerosis (ALS), better known as Lou Gehrig’s disease, acts. Working with a powerful fruit fly model of the disease, they found a way of reducing disease toxicity that slows the dysfunction of neurons, while showing that a parallel mechanism can reduce toxicity in mammalian cells. Their discoveries offer the possibility of a new strategy for treating ALS. The only drug treatment currently available extends life spans by just three months on average.
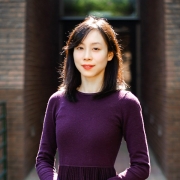
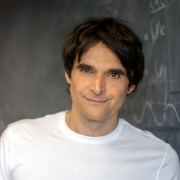
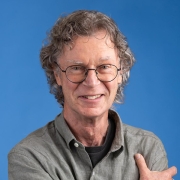
The senior author of the study is Nancy Bonini, Florence R.C. Murray Professor of Biology. Contributors from her lab include Hyung-Jun Kim, Leeanne McGurk, and Ross Weber. They partnered on the work with long-time collaborators from the Perelman School of Medicine, John Trojanowski and Virginia M-Y Lee. Additional co-authors included Alya Raphael and Aaron Gitler of Stanford University and Eva LaDow and Steven Finkbeiner of the Gladstone Institute of Neurological Disease.
A key gene, TDP-43, has recently come to light as playing a role in the disease. Using yeast models and fruit flies, the team showed that genes that modulate cellular structures known as stress granules, which act as holding pens for RNA and proteins when cells are under stress, modify TDP-43 toxicity. Previous work had suggested that ALS patients may have abnormal accumulations of stress granule components, indicating that the structures might somehow be tied to the disease. In flies, the Bonini team found that expression of genes predicted to promote stress granules increased the toxic activity of TDP-43 in genetic screens, underlining the importance of these structures to the pathology of ALS.
Investigating fruit flies engineered to express the human version of TDP-43, they found the flies showed signs of a build-up of stress granule components. The researchers were able to modulate symptoms reflective of ALS by altering the expression of genes related to stress granules.
Further, using transgenic flies, the team identified a region of ataxin-2—a gene that interacts with TDP-43 and whose mutations can cause degenerative diseases on its own—is critical to increasing the detrimental effects of TDP-43. By knocking out this region of ataxin-2, which is known to contribute to stress granules, they were able to dramatically reduce the interaction between TDP-43 and ataxin-2. The information suggests that the disease state may be associated with pathological stress granules, possibly remaining in the cell too long or not being resolved properly.
Finally, the researchers went back to the fly to see if they could reverse TDP-43 toxicity. Upon feeding flies a compound that is predicted to mitigate stress granules, they witnessed a dramatic restoration of physical strength in the flies expressing TDP-43. Those fed the compound retained more climbing ability compared with flies without the compound. The team then ran successful tests on mammalian cells.
The results show promise for a treatment strategy for ALS, and highlight again the power that simple model organisms can have in shedding light on human neurological disease.
The study was funded by the National Institutes of Health, the Howard Hughes Medical Institute, the Robert Packard Center for ALS, the Williams H. Adams Foundation, Target ALS, and a BrightFocusAlzheimer’s disease grant.
Read the full story here.